Questioning Routine in Diagnostic Practices
In the world of healthcare, laboratory tests are indispensable tools, providing crucial insights for diagnosis and treatment. However, the sheer volume of available tests can sometimes lead to a phenomenon: the over-ordering of certain labs, often driven by habit or a desire for comprehensive data, even when the clinical need is less clear.
While well-intentioned, this practice can lead to unnecessary costs, patient anxiety, and potentially misleading results. Let’s explore some of the most frequently over-ordered lab tests and when their utility might be more limited.
The Routine CBC (Complete Blood Count) Without Specific Indication
The CBC is a common test ordered during routine physicals, often as a broad screen of overall health.
While the CBC provides valuable information about blood cell counts and can detect various conditions, ordering it indiscriminately in asymptomatic individuals with no specific risk factors may yield limited actionable insights. Abnormalities found incidentally often require further, potentially invasive, investigations.
The CBC is undoubtedly essential for patients presenting with symptoms like fatigue, unexplained bruising, fever, or suspected infection. It’s also crucial for monitoring patients with hematological disorders or undergoing certain treatments. However, for healthy individuals without specific complaints, its routine annual ordering may not always be necessary.
The Broad Vitamin D Screening
Vitamin D testing has become increasingly popular, fueled by awareness of its importance in various bodily functions.
While vitamin D deficiency is a concern for certain populations (e.g., those with limited sun exposure, malabsorption issues, or specific medical conditions), widespread screening of the general population without risk factors is debated. Evidence supporting routine supplementation based solely on screening results in low-risk individuals is not robust.
Testing for vitamin D levels is most beneficial in individuals with symptoms suggestive of deficiency (e.g., bone pain, muscle weakness), those with known risk factors, or when monitoring response to supplementation.
The Comprehensive Metabolic Panel (CMP) for Everyone
The CMP, which includes tests for electrolytes, kidney function, liver enzymes, and glucose, is another frequent component of routine check-ups.
Similar to the CBC, the CMP offers a broad overview. However, in the absence of specific symptoms or risk factors for metabolic or organ dysfunction, the likelihood of uncovering clinically significant findings through routine annual testing in healthy individuals is relatively low.
Ordering individual components of the CMP (e.g., creatinine for kidney function in high-risk individuals, liver enzymes in those with a history of liver disease or alcohol use) based on clinical suspicion or risk factors is often a more targeted and efficient approach.
Thyroid Function Tests (TSH) as a Universal Screen
Thyroid-stimulating hormone (TSH) testing is often included in general health panels.
While thyroid disorders are relatively common, routine screening of asymptomatic individuals for thyroid dysfunction has not consistently demonstrated improved outcomes. Over-testing can lead to the detection of subclinical abnormalities, which may not require treatment and can cause unnecessary anxiety.

TSH testing is clearly indicated in patients with symptoms suggestive of thyroid disease (e.g., fatigue, weight changes, hair loss), those with a family history of thyroid disorders, or individuals with certain autoimmune conditions.
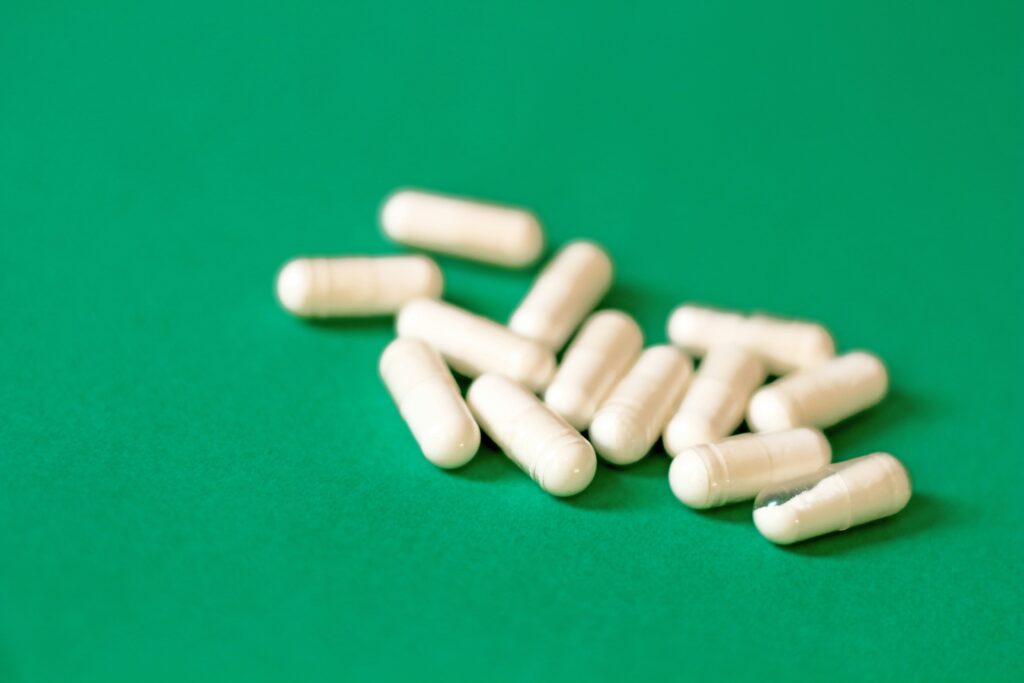
The over-ordering of lab tests carries several potential downsides. It contributes to increased healthcare costs, can lead to false-positive results that trigger further unnecessary and potentially invasive procedures, and can generate anxiety for patients awaiting results for non-significant findings.
Prostate-Specific Antigen (PSA) for Universal Prostate Cancer Screening
For many years, annual PSA testing was a common recommendation for prostate cancer screening in men of a certain age.
Current guidelines have shifted due to evidence suggesting that routine PSA screening in all men can lead to over-diagnosis of slow-growing cancers that may never cause harm, resulting in unnecessary anxiety and treatment with potential side effects.

The focus is now on a more individualized approach, considering factors like age, family history, race, and individual preferences. Discussions about the potential benefits and risks of PSA testing are crucial, rather than a blanket recommendation for all men. Testing is more clearly indicated for those with specific risk factors or symptoms.
Comprehensive Allergy Panels for Non-Specific Symptoms
When individuals experience vague symptoms like fatigue, headaches, or gastrointestinal issues, a comprehensive allergy panel is sometimes ordered to identify potential triggers.
While these panels test for a wide range of allergens (foods, environmental factors, etc.), a positive result doesn’t always correlate with a true clinical allergy causing the specific symptoms. Many people can have positive IgE antibodies to certain substances without experiencing any allergic reactions upon exposure (sensitization without allergy).

Diagnosing allergies should primarily be based on a detailed clinical history, including the timing and nature of symptoms in relation to potential exposures. Targeted allergy testing, guided by the patient’s history, or supervised oral food challenges are often more informative than broad screening panels for non-specific symptoms. A positive result on a comprehensive panel requires careful interpretation in the context of the patient’s actual experiences.
Moving Towards Judicious Testing
Promoting a more thoughtful approach to lab test ordering involves several key aspects:

- Evidence-Based Guidelines: Adhering to clinical guidelines that outline appropriate testing indications.
- Shared Decision-Making: Engaging in conversations between clinicians and patients about the rationale for each test.
- Focus on Individual Risk Factors and Symptoms: Tailoring test selection based on a patient’s specific medical history, risk factors, and presenting complaints.
- Regular Review of Testing Practices: Healthcare systems should periodically evaluate their testing patterns to identify areas of potential over-utilization.
Prioritizing Purposeful Testing
Laboratory tests are powerful diagnostic aids, but their value is maximized when used strategically and based on clinical necessity. By questioning routine practices and focusing on individualized patient needs, we can move towards a more efficient and patient-centered approach to diagnostic testing, ensuring that these valuable tools are used effectively and responsibly.